Introduction
Physical therapy in Downtown Birmingham and onsite at American Cast Iron and Pipe for Myositis Ossificans
Welcome to Iron City Physical Therapy’s resource on Myositis Ossificans.
A muscle strain or muscle contusion (bruise) can sometimes result in an unfortunate complication called myositis ossificans (MO). With this injury, cells within the belly of the muscle start to ossify (turn to bone).
This guide will help you understand:
- the anatomy of a muscle
- what myositis ossificans is
- the symptoms of myositis ossificans
- how your health care professional diagnoses myositis ossificans
- what Iron City Physical Therapy’s approach to rehabilitation is
Anatomy
What parts of the body are involved?
Muscles are composed of many fibers bundled together; the bigger, more frequently used muscles have more fibers than the smaller, lesser-used ones. The muscle fibers are made up of smaller muscle-type cells.
Among the muscles are voluntary and involuntary muscles. Voluntary, or skeletal muscles, are those that we move by choice (for example, the muscles in your arms and legs). Involuntary muscles, or smooth muscles, are the ones that move on their own (for example, the muscles that control your diaphragm and help you breathe). The muscles in your heart are called involuntary cardiac muscles.
Skeletal muscles are attached to bones both by tendons at either end of the bone, which is a sinewy type of tissue. The muscle is also attached directly onto the outside lining of the bone itself, which is called the periosteum.
MO occurs in the skeletal muscles of the body, and most often in the large muscles of the upper and lower extremities, such as the biceps of the upper arm or the quadriceps muscle of the thigh, but it can occur in any of the skeletal muscles.
Causes
MO can be divided into two main types. The first, which is usually related to a specific traumatic event or injury to a muscle, is termed myositis ossificans traumatica or traumatic MO. Interestingly enough, however, with this type of MO there are times when an exact injury or trauma actually can’t be identified and a repeated microtrauma may be suspected.
The second type of MO is called myositis ossificans progressiva, which is actually an inherited condition and is different from that which occurs in the process of myositis ossificans traumatica. This type of MO will not be discussed in this patient guide.
Traumatic MO, which is the topic of this patient guide, results in what is termed heterotrophic ossification. Heterotrophic ossification means that bone has formed in a part of the anatomy where it usually does not form, such as soft tissue. Heterotrophic ossification can occur for a number of reasons. MO falls under the category of a type of heterotrophic ossification in which the abnormal bone forms within muscle.
Exactly why MO occurs is not agreed upon. It is theorized to occur as a result of an injury to the muscle, which may also affect the outside of the bone that the muscle is attached to (the periosteum). This trauma either allows bone cells from the periosteum to enter into the muscle and start to grow where they should not, or causes basic cells within the muscle to turn into bone-forming cells.
Although the exact mechanism of bone formation is not known, it is widely accepted that there are a few factors that increase the likelihood of MO forming. These include having sustained a more severe injury, a severe loss of range of motion after the injury, injuries that are massaged too aggressively early on in their healing, injuries that are subject to aggressive activity before they are ready, and injuries that get re-injured before they have fully healed.
Symptoms
Because MO is not considered to have arisen until actual bone formation (calcification) has occurred, MO is generally not diagnosed until a minimum of 2 weeks after an injury, as this is the least amount of time it takes for bone formation to occur and to be seen on plain x-ray. Often it takes 3-6 weeks for the bone calcification to show up and MO is not officially diagnosed until the bone formation is seen on x-ray or other investigation. By the time bone formation has occurred, symptoms may include a palpable lump in the muscle, range of motion that is more restricted than it should be, weakness of the muscle, and ongoing pain. Leading up to the bone formation, the symptoms of MO present initially as the typical symptoms of a muscle injury, and include pain, a limited range of motion, weakness, and bruising in the area or down the limb. A lump in the muscle felt earlier than 2-3 weeks post injury is likely a hematoma, which is the pooling of blood from the injury.
At the time that most muscle injuries should be improving, those with MO show no improvement in their pain or range of motion. A palpable mass may be felt in the muscle and they may be limited in the function of their limb, including walking with a limp if the injury is in their lower extremity. Patients with MO may develop significant pain after using the muscle, or may have pain during the night or upon waking up. Most patients experience normal initial rehabilitation and show improvement in their symptoms early on in their recovery but then this improvement either halts or deteriorates as the bone forms.
If your physical therapist suspects MO, they will send you to your physician so that the proper diagnostic tests can be done to confirm the diagnosis.
Diagnosis
A good history of your injury may be enough for your health care professional to suspect MO. MO, however, is not confirmed as a diagnosis until calcified bone is seen on a diagnostic test such as an x-ray, a computed tomography scan (CT), an ultrasound, bone scan, or a magnetic resonance image (MRI). In most cases, only an x-ray is required but other tests, including a muscle biopsy may be used to confirm a diagnosis or when further investigation is required.
As stated previously, MO does not occur immediately after an injury, but rather occurs over time. In most cases a minimum of 2 weeks, but often 3-4 weeks is required before the calcified bone shows up on an x-ray. In the early time frame after an injury (0-2 weeks) a diagnosis of MO is not possible, however factors that can increase the likelihood of MO developing over time can be monitored during the early post-injury period.
Rehabilitation
Physical therapy at Iron City Physical Therapy can be very useful in treating MO, but the most useful therapy is prevention of MO occurring in the first place!
If you sustain a muscle strain or contusion, seek proper care and advice from your physical therapist at Iron City Physical Therapy in the treatment of this injury. Poor care including activity or self-treatment which is too aggressive, can increase your chances of developing MO. Heed the advice given to you by your physical therapist and check in regularly with them so they can monitor your rehabilitation and watch for signs indicating that your injury is not improving as it typically should, which may indicate that MO is developing.
MO can develop due to poor or aggressive care of an injury, but for some unlucky individuals it can also occur even with the proper care and treatment provided. In these cases focus needs to turn to providing the appropriate care to the injury once the MO has been confirmed.
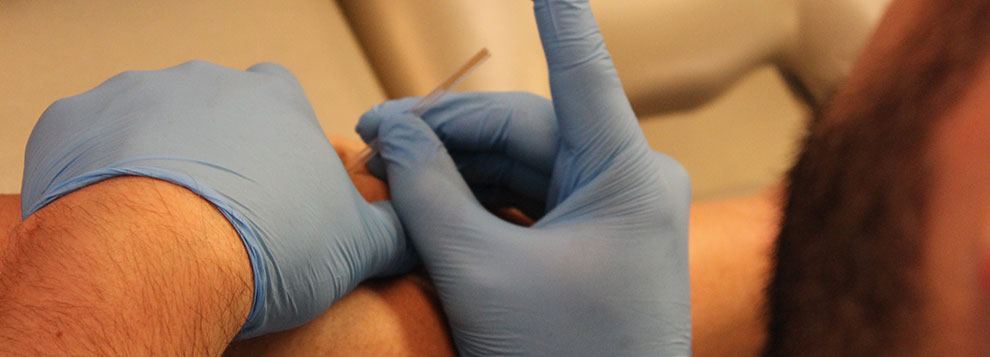
Your physical therapist at Iron City Physical Therapy can guide you through the appropriate rehabilitation to recover from MO. Initial treatment will focus on decreasing your pain. Your therapist may use modalities such as ultrasound, interferential current, transcutaneous electrical nerve stimulation, ice, heat, or other modalities to ease your pain. They may also use some gentle massage to the injured muscle both for pain relief and to encourage mobility of the tissues and the limb. Aggressive massage directly over the area can cause further injury if the bone hasn’t fully ossified so your therapist will take caution when doing so. This treatment is best reserved for once it has been confirmed that the boney growth is no longer proliferating, which your doctor can confirm from the diagnostic tests that have been done.
Rest from aggravating activities will be an important part of your treatment as well. Your therapist will advise you against any activity that brings on pain. They will prescribe gentle stretching exercises to help preserve your current range of motion and slowly assist you to gain further range. Pain during stretching should be heeded and not pushed passed. Your therapist will review the limits of your stretching to ensure you are not being too aggressive, which can hinder your recovery.
In addition to stretching, your therapist will prescribe gentle strengthening exercises. Initially these exercises may only consist of simply tightening your muscle without moving your limb (isometric exercise) but gradually as you recover and gain more range of motion, more intensive exercises will be prescribed. When appropriate, exercises that assist you to return to your normal activities both for work and play will be incorporated into your rehabilitation.
In addition to physical therapy treatment, anti-inflammatory medication may be useful in some cases to assist with the MO healing process. Your doctor will determine if and when this may be most useful in your individual case.
Over time the body usually either naturally reabsorbs the boney tissue that has formed or the boney tissue remains present but full range of motion and strength is gained and the body just works around the now permanent boney tissue within the muscle. In some unfortunate cases, despite appropriate rehabilitation, pain in the muscle remains and range of motion and strength cannot be progressed. In these cases your physical therapist will suggest that you see an orthopaedic surgeon as surgical treatment will need to be considered.
Surgery
Although surgery is a rare necessity in cases of MO, there are times when it may be required to excise the boney tissue that has formed. These cases include those that have not responded to physical therapy treatment and remain painful and have poor range of motion and strength. Other cases include those where the boney tissue is close to a joint and is restricting its motion, or cases where it is close to a nerve and causing irritation to the nerve.
When surgical bone excision is required it is necessary that the bone tissue has fully matured before it is excised or it could reoccur. Repeated x-rays or other diagnostic tests that are closely examined by your surgeon will help him or her determine whether the tissue is ready for excision. Post-surgical physical therapy at Iron City Physical Therapy should be done and will focus on decreasing any new pain from the surgery, regaining your maximum range of motion and strength, and assisting you to return back to your regular activities within an appropriate time frame.
Conclusion
MO is a serious complication related to a muscle strain, contusion, or repeated microtrauma to a muscle. Proper initial care of the original muscle injury is crucial in avoiding MO, but if it does occur, physical therapy at Iron City Physical Therapy can assist you to recover and regain your full range of motion and strength without any further complications.