Introduction
Physical therapy in Downtown Birmingham and onsite at American Cast Iron and Pipe for Foot
Welcome to Iron City Physical Therapy's patient resource about Plantar Fasciitis (Heel Pain).
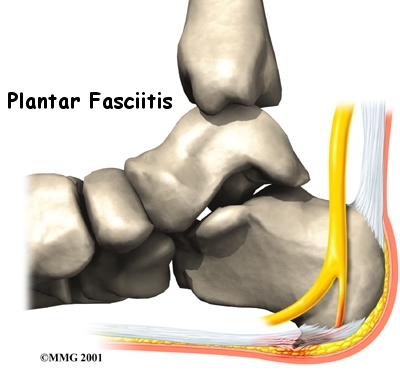
Plantar fasciitis is a painful condition affecting the bottom of the foot. It is a common cause of heel pain and is sometimes called a heel spur. Plantar fasciitis is the correct term to use when there is active inflammation. Plantar fasciosis is more accurate when there is no inflammation but chronic degeneration instead. Acute plantar fasciitis is defined as inflammation of the origin of the plantar fascia and fascial structures around the area. Plantar fasciitis or fasciosis is usually just on one side. In about 30 per cent of all cases, both feet are affected.
This article will help you understand:
- how plantar fasciitis develops
- how the condition causes problems
- what can be done for your pain
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Foot therapy|limit:15|heading:Hear from some of our *Foot Therapy* patients#
Anatomy
Where is the plantar fascia, and what does it do?
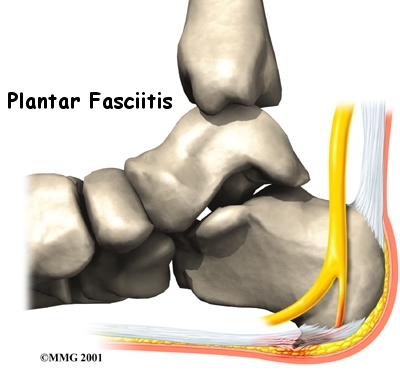
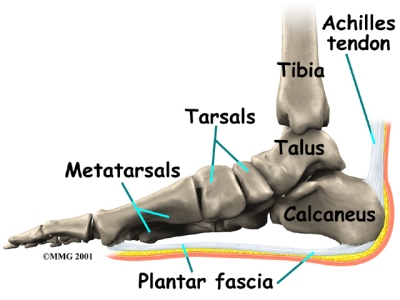
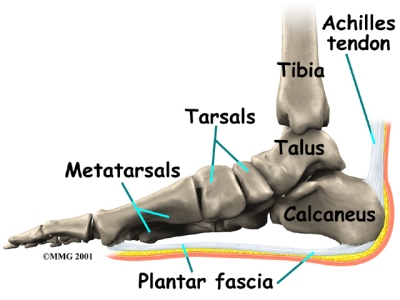 The (also known as the plantar aponeurosis) is a thick band of connective tissue. It runs from the front of the heel bone (calcaneus) to the ball of the foot. This dense strip of tissue helps support the arch of the foot by acting something like the string on an archer's bow. It is the source of the painful condition plantar fasciitis.
The (also known as the plantar aponeurosis) is a thick band of connective tissue. It runs from the front of the heel bone (calcaneus) to the ball of the foot. This dense strip of tissue helps support the arch of the foot by acting something like the string on an archer's bow. It is the source of the painful condition plantar fasciitis.
The plantar fascia is made up of collagen fibers oriented in a lengthwise direction from toes to heel (or heel to toes). There are three separate parts: the medial component (closest to the big toe), the central component, and the lateral component (on the little toe side). The central portion is the largest and most prominent.
Both the plantar fascia and the Achilles' tendon attach to the calcaneus. The connections are separate in the adult foot. Although they function separately, there is an indirect relationship. If the toes are pulled back toward the face, the plantar fascia tightens up. This position is very painful for someone with plantar fasciitis. Force generated in the Achilles’ tendon increases the strain on the plantar fascia. This is called the windlass mechanism. Later, we’ll discuss how this mechanism is used to treat plantar fasciitis with stretching and night splints.
Related Document: Iron City Physical Therapy's Guide to Foot Anatomy
Causes
How does plantar fasciitis develop?
Plantar fasciitis can come from a number of underlying causes. Finding the precise reason for the heel pain is sometimes difficult.
 As you can imagine, when the foot is on the ground a tremendous amount of force (the full weight of the body) is concentrated on the plantar fascia. This force stretches the plantar fascia as the arch of the foot tries to flatten from the weight of your body. This is just how the string on a bow is stretched by the force of the bow trying to straighten. This leads to stress on the plantar fascia where it attaches to the heel bone. Small tears of the fascia can result. These tears are normally repaired by the body.
As you can imagine, when the foot is on the ground a tremendous amount of force (the full weight of the body) is concentrated on the plantar fascia. This force stretches the plantar fascia as the arch of the foot tries to flatten from the weight of your body. This is just how the string on a bow is stretched by the force of the bow trying to straighten. This leads to stress on the plantar fascia where it attaches to the heel bone. Small tears of the fascia can result. These tears are normally repaired by the body.
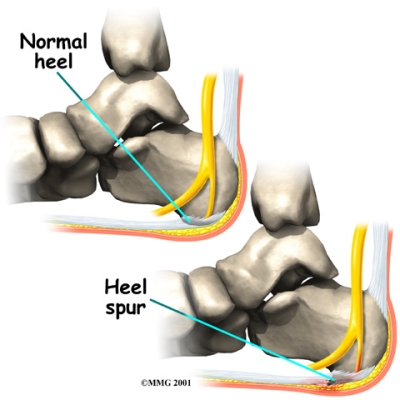
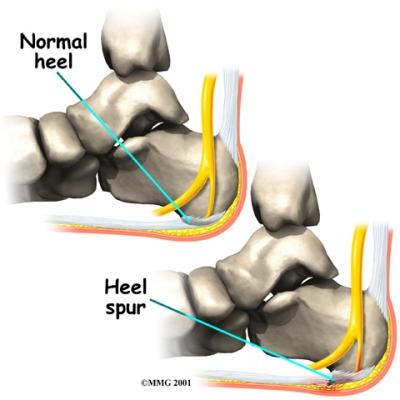
As this process of injury and repair repeats itself over and over again, (a pointed outgrowth of the bone) sometimes forms as the body's response to try to firmly attach the fascia to the heelbone. This appears on an X-ray of the foot as a heel spur. Bone spurs occur along with plantar fasciitis but they are not the cause of the problem.
As we age, the very important that makes up the fleshy portion of the heel becomes thinner and degenerates (starts to break down). This can lead to inadequate padding on the heel. With less of a protective pad on the heel, there is a reduced amount of shock absorption. These are additional factors that might lead to plantar fasciitis.
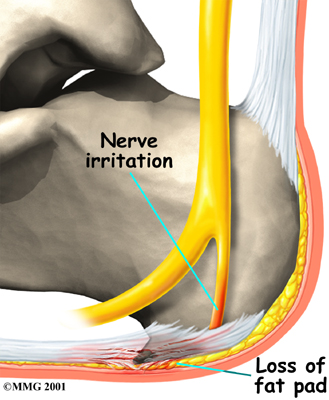
Some physicians feel that the small nerves that travel under the plantar fascia on their way to the forefoot become irritated and may contribute to the pain. But some studies have been able to show that pain from compression of the nerve is different from plantar fasciitis pain. In many cases, the actual source of the painful heel may not be defined clearly.
Symptoms
What does plantar fasciitis feel like?
The symptoms of plantar fasciitis include pain along the inside edge of the heel near the arch of the foot. The pain is worse when weight is placed on the foot. This is usually most pronounced in the morning when the foot is first placed on the floor.
Prolonged standing can also increase the painful symptoms. It may feel better after activity but most patients report increased pain by the end of the day. Pressing on this part of the heel causes tenderness. Pulling the toes back toward the face can be very painful.
Diagnosis
How do health care providers diagnose the condition?
When you first visit Iron City Physical Therapy, our physical therapist will examine your foot and speak with you about the history of your problem. Diagnosis of plantar fasciitis is generally made during the history and physical examination. There are several conditions that can cause heel pain, and plantar fasciitis must be distinguished from these conditions.
Some patients may be referred to a doctor for further diagnosis. Once your diagnostic examination is complete, the physical therapists at Iron City Physical Therapy have treatment options that will help speed your recovery, so that you can more quickly return to your active lifestyle.
Our Treatment
Non-surgical Rehabilitation
Nonsurgical management of plantar fasciitis is successful in 90 per cent of all cases. When you begin therapy at Iron City Physical Therapy, our physical therapist will design exercises to improve flexibility in the calf muscles, Achilles' tendon, and the plantar fascia.
We will apply treatments to the painful area to help control pain and swelling. Examples include ultrasound, ice packs, and soft-tissue massage. Our physical therapy sessions sometimes include iontophoresis, which uses a mild electrical current to push anti-inflammatory medicine, prescribed by your doctor, into the sore area.
We may have a customized arch support, or orthotic, designed to support the arch of your foot and to help cushion your heel. Supporting the arch with a well fitted orthotic may help reduce pressure on the plantar fascia. Alternatively, we may recommend placing a special type of insert into the shoe, called a heel cup. This device can also reduce the pressure on the sore area. Wearing a silicone heel pad adds cushion to a heel that has lost some of the fat pad through degeneration.
Your physical therapist will also provide ideas for therapies that you can perform at home, such as doing your stretches for the calf muscles and the plantar fascia. We may also have you fit with a night splint to wear while you sleep. The night splint keeps your foot from bending downward and places a mild stretch on the calf muscles and the plantar fascia. Some people seem to get better faster when using a night splint and report having less heel pain when placing the sore foot on the ground in the morning.
We find that many times it takes a combination of different approaches to get the best results for patients with plantar fasciitis. There isn’t a one-size-fits-all plan. Some patients do best with a combination of heel padding, medications, and stretching. If this doesn’t provide relief from symptoms within four to six weeks, then we may advise additional physical therapy and orthotics.
Finding the right combination for you may take some time. Don't be discouraged if it takes a few weeks to a few months to find the right fit for you. Most of the time, the condition is self-limiting. This means it doesn't last forever but does get better with a little time and attention. But in some cases, it can take up to a full year or more for the problem to be resolved.
Post-surgical Rehabilitation
Although recovery rates vary among patients, it generally takes several weeks before the tissues are well healed after surgery. The incision is protected with a bandage or dressing for about one week after surgery. You will probably use crutches briefly, and your physical therapist can help you learn to properly use your crutches to avoid placing weight of your foot while it heals.
The stitches are generally removed in 10 to 14 days. However, if your surgeon used sutures that dissolve, you won't need to have the stitches taken out. You should be released to full activity in about six weeks.
Surgical release of the plantar fascia decreases stiffness in the arch. However, it can also lead to collapse of the longitudinal (lengthwise) arch of the foot. Releasing the fascia alters the biomechanics of the foot and may decrease stability of the foot arch. The result may be increased stress on the other plantar ligaments and bones. Fractures and instability have been reported in up to 40 per cent of patients who have a plantar fasciotomy.
Throughout your post-surgical recovery, our physical therapist will note your progress and be watchful for the development of fractures and instability. When your recovery is well under way, regular visits to Iron City Physical Therapy will end. Although we will continue to be a resource, you will eventually be in charge of doing some therapeutic exercises as part of an ongoing home program.
Iron City Physical Therapy provides services for physical therapy in Downtown Birmingham and onsite at American Cast Iron and Pipe.
Physician Review
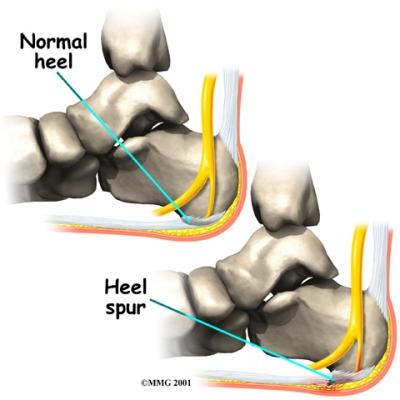 Your doctor may order an X-ray to rule out a stress fracture of the heel bone and to see if a is present that is large enough to cause problems. Other helpful imaging studies include bone scans, MRI, and ultrasound. Ultrasonographic exam may be favored as it is quick, less expensive, and does not expose you to radiation.
Your doctor may order an X-ray to rule out a stress fracture of the heel bone and to see if a is present that is large enough to cause problems. Other helpful imaging studies include bone scans, MRI, and ultrasound. Ultrasonographic exam may be favored as it is quick, less expensive, and does not expose you to radiation.
Laboratory investigation may be necessary in some cases to rule out a systemic illness causing the heel pain, such as rheumatoid arthritis, Reiter's syndrome, or ankylosing spondylitis. These are diseases that affect the entire body but may show up at first as pain in the heel.
A cortisone injection into the area of the fascia may be used but has not been proven effective. Studies show better results when ultrasound is used to improve the accuracy of needle placement. Cortisone should be used sparingly since it may cause rupture of the plantar fascia and fat pad degeneration and atrophy, making the problem worse.
Botulinum toxin A, otherwise known as BOTOX, has been used to treat plantar fasciitis. The chemical is injected into the area and causes paralysis of the muscles. BOTOX has direct analgesic (pain relieving) and antiinflammatory effects. In studies so far, there haven’t been any side effects of this treatment.
Shock wave therapy is a newer form of nonsurgical treatment. It uses a machine to generate shock wave pulses to the sore area. Patients generally receive the treatment once each week for up to three weeks. It is not known exactly why it works for plantar fasciitis. It's possible that the shock waves disrupt the plantar fascial tissue enough to start a healing response. The resulting release of local growth factors and stem cells causes an increase in blood flow to the area. Recent studies indicate that this form of treatment can help ease pain, while improving range of motion and function.
Clinical trials are underway investigating the use of radiofrequency to treat plantar fasciitis. It is a simple, noninvasive form of treatment. It allows for rapid recovery and pain relief within seven to 10 days. The radio waves promote angiogenesis (formation of new blood vessels) in the area. Once again, increasing blood flow to the damaged tissue encourages a healing response.
Antiinflammatory medications are sometimes used to decrease the inflammation in the fascia and reduce your pain. Studies show that just as many people get better with antiinflammatories as those who don't have any improvement. Since these medications are rarely used alone, it's difficult to judge their true effectiveness.
Surgery
Surgery is a last resort in the treatment of heel pain. Physicians have developed many procedures in the last 100 years to try to cure heel pain. Most procedures that are commonly used today focus on several areas:
- remove the bone spur (if one is present)
- release the plantar fascia (plantar fasciotomy)
- release pressure on the small nerves in the area
Usually the procedure is done through a small incision on the inside edge of the foot, although some surgeons now perform this type of surgery using an endoscope. An endoscope is a tiny TV camera that can be inserted into a joint or under the skin to allow the surgeon to see the structures involved in the surgery. By using the endoscope, a surgeon can complete the surgery with a smaller incision and presumably less damage to normal tissues. It is unclear whether an endoscopic procedure for this condition is better than the traditional small incision.
Surgery usually involves identifying the area where the plantar fascia attaches to the heel and releasing the fascia partially from the bone. If a small spur is present that is removed. The small nerves that travel under the plantar fascia are identified and released from anything that seems to be causing pressure on the nerves. This surgery can usually be done on an outpatient basis. This means you can leave the hospital the same day.
Portions of this document copyright MMG, LLC.




 The
The 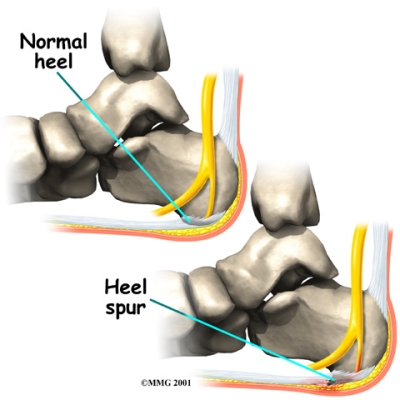 As you can imagine, when the foot is on the ground a tremendous amount of force (the full weight of the body) is concentrated on the plantar fascia. This force stretches the plantar fascia as the arch of the foot tries to flatten from the weight of your body. This is just how the string on a bow is stretched by the force of the bow trying to straighten. This leads to stress on the plantar fascia where it attaches to the heel bone. Small tears of the fascia can result. These tears are normally repaired by the body.
As you can imagine, when the foot is on the ground a tremendous amount of force (the full weight of the body) is concentrated on the plantar fascia. This force stretches the plantar fascia as the arch of the foot tries to flatten from the weight of your body. This is just how the string on a bow is stretched by the force of the bow trying to straighten. This leads to stress on the plantar fascia where it attaches to the heel bone. Small tears of the fascia can result. These tears are normally repaired by the body.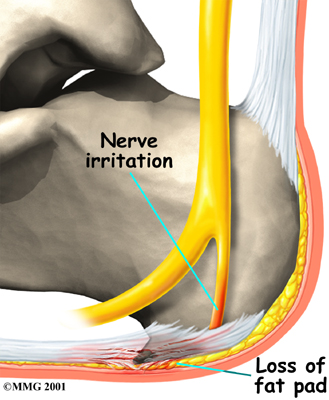
 Your doctor may order an X-ray to rule out a stress fracture of the heel bone and to see if a
Your doctor may order an X-ray to rule out a stress fracture of the heel bone and to see if a 